Man whose heart stopped for three hours makes full recovery
25 June 2021 - Patient flown to King’s College Hospital for life-saving ‘blood warming’ treatment after being submerged in near-freezing waters
A patient whose heart stopped beating for more than three hours has made a full recovery thanks to a “chain of survival” that resulted in rapid access to an artificial heart and lung machine.
In April, Paul Curtis was flown to King’s College Hospital and put on extracorporeal membrane oxygenation (ECMO) – a machine that takes over the work of the lungs and heart – after a kayaking accident in Maidstone left him in submerged in near-freezing waters for around five minutes, causing life-threatening hypothermia.
The 50-year-old accountant and recreational endurance athlete from Gillingham initially managed to get out of the water but with his core body temperature dropping to just 23 degrees his heart began to quiver and stopped pumping blood. Following his collapse in the local clubhouse a friend who had been out kayaking with him at the time of the accident administered cardiopulmonary resuscitation (CPR) before the ambulance service arrived and took over.
With Paul’s core body temperature so low, paramedics were unable to shock his heart into a normal rhythm so Air Ambulance Kent Surrey Sussex was called to ensure a rapid transfer to King’s. While in the air, a mechanical chest compression system kept Paul alive before he was transferred onto the ECMO machine, which warmed his body.
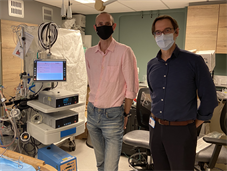
Dr Georg Auzinger, Consultant in Critical Care and Director of the ECMO Service at King’s, said, “Normal body temperature is around 36 to 37 degrees but Paul’s dropped down to just 23 degrees, causing his heart to stop beating in a rhythm that could sustain life. Although he had no cardiac output for more than three hours, thankfully, Paul received the necessary first aid both at the scene and on his way to King’s to ensure his brain was not starved of oxygen. Once at King’s we used extracorporeal membrane oxygenation (ECMO) to supply Paul’s vital organs, and especially his brain, with oxygen and warm the blood.
“ECMO is a type of long-term artificial heart-lung machine, which pumps blood around the body, adding oxygen and removing carbon dioxide, just like the heart and lungs would do. The machine rewarms the blood and returns it to the body, and this enabled us to shock Paul’s heart back into a normal rhythm.”
Speaking from his hospital bed, Paul said, “The care I’ve had pre-hospital and at King’s has been phenomenal. The fact that I’m here today is testament to the skill and dedication of everyone who cared for me.” Paul, who has taken part in triathlons, iron man events and ultra-marathons, is unsure about whether he will return to the water. “I’ve been given a second chance so I have to think carefully about whether I’ll kayak again,” he added.
Paul’s partner Christine Cordle, a community nurse, said, “It’s a miracle Paul is with us today. If just one link in Paul’s chain of survival – which included his friend who first administered CPR, the paramedics, air ambulance, A&E and critical care unit at King’s – had broken he wouldn’t be with us now.”
King’s is one of a small number of centres in the country with an established ECMO service. Set up in 2012, it requires specialist equipment and clinical expertise. Around 150 patients at King’s have been supported by ECMO, including children and adults with liver failure, who have been successfully bridged to life saving liver transplants, and COVID patients.
