New life-saving approach to liver transplant developed at King’s College Hospital
14 October 2024 - A team at King’s have helped ensure patients with an often fatal liver condition are now a priority transplant group
People living with acute-on-chronic liver failure (ACLF) are now being prioritised for life-saving liver transplants, following work at King’s College Hospital to treat patients with the condition.
ACLF is a serious condition that happens when someone with long term liver disease develops organ failure. Patients were previously rarely considered for a liver transplant because of how suddenly and quickly people become severely ill. They often quickly became too ill to survive a transplant, or died before a suitable donor could be found.
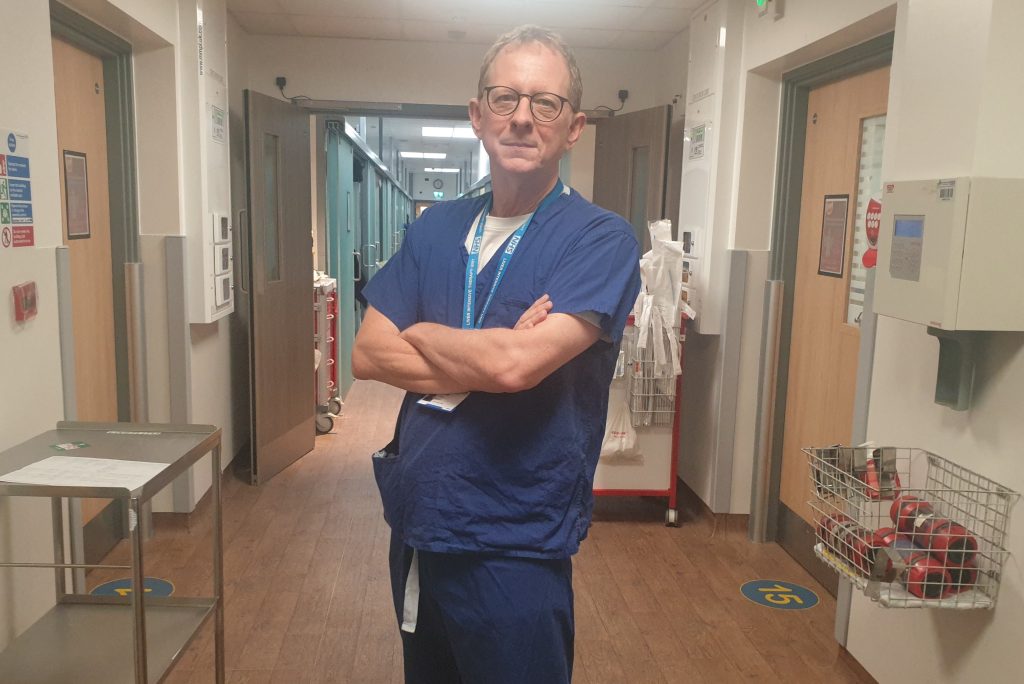
However, a new service, led by Professor William Bernal of the Liver Intensive Therapy Unit at King’s, has found that when these patients were made one of the UK’s national priority groups for transplantation, more than three quarters (77%) of people with ACLF who were transplanted were still alive one year later.
This is the first time critically ill patients with ACLF have been prioritised in a planned national transplant programme. This is also the first time liver transplant has been shown to be a practical and highly effective treatment for selected patients with ACLF when no other treatment option existed.
A service evaluation was launched in 2021 which prioritised ACLF patients immediately after super-urgent patients, but before the elective tier, and this became standard practice at the end of 2023. Details have this week been published in the scientific journal, Lancet Regional Health Europe, and the life-saving approach is now being considered by other countries across the world.
Professor Bernal, lead author of the Lancet paper, developed the service and worked with other clinicians across the country to deliver the pilot on behalf of the NHS Blood and Transplant Liver Advisory Group. He said: “As a doctor working in a liver intensive care unit I was used to seeing the devastating impact of this condition. It was truly heart-breaking to see young people come into the unit with multiple organ failure and as a doctor have very few options to keep them alive.
“These patients now have access to a lifesaving therapy for the first time. I feel a sense of pride at seeing the results.
“There is an urgent clinical need for interventions to improve survival for people with this disease, which causes many of the two million deaths from chronic liver disease world-wide each year.”
Professor Derek Manas, the Medical Director of Organ and Tissue Donation and Transplantation at NHS Blood and Transplant said: “The success of this change is a tribute to the work of the whole liver transplant community. People with ACLF are critically ill – even with prioritisation, nearly 20% of people in the pilot service died before transplantation was possible.
“The results confirm that for carefully selected ACLF patients, liver transplantation is a practical and highly effective treatment option where no other similarly effective interventions exist. But without the generosity of donor families no transplants are possible – we urge people to show their support on the NHS Organ Donor Register.”
NHSBT introduced the changes following work by the NHSBT Liver Advisory Group and the UK’s seven liver transplant centres. The Lancet paper published today was written by King’s College Hospital and NHSBT with the seven liver transplant centres.
Of the 52 patients ACLF patients listed for transplant during the pilot phase, 42 received transplants and 77% were alive one year later. By comparison, all 10 of the people who did not receive transplants sadly died within 13 days.
ACLF can affect people of any age but the patient group is younger than average for many illnesses. The people listed for transplant during the evaluation were aged between 39 to 52 years old.
King’s is one of the busiest liver centres in the country, carrying out over 200 adult and child transplant operations every year.
